Insurance companies may now consider bariatric surgery
Insurance coverage

New guidelines say surgery should also be considered for some mildly obese people with diabetes and a BMI between 30 and 40.
Recent guidelines recommending bariatric surgery for obese people with Type 2 diabetes could convince more insurance companies to green-light the procedure.
“I think these guidelines will encourage insurers to provide coverage for this kind of surgery for some diabetic patients who are having so much trouble maintaining their sugar levels,” said Timothy J. Gardner, medical director of the Center for Heart and Vascular Health at Christiana Care Health System in Delaware.
“Insurers tend to go with the evidence, and this group of experts provided a lot of really important evidence,” he said.
A recent joint statement endorsed by 45 international professional organizations, researchers and clinicians urged doctors to recommend bariatric surgery as a treatment option for certain obese people with diabetes who have failed to respond to conventional treatment. The American Heart Association was not involved in the consensus development or treatment algorithm.
The article, titled Metabolic Surgery in the Treatment Algorithm for Type 2 Diabetes: A Joint Statement by International Diabetes Organizations, appeared May 24 in Diabetes Care.
“I suspect the insurance coverage is going to expand to cover the surgeries as the guidelines are recommending now … but we need more data on cost effectiveness,” said Dr. Francisco Lopez-Jimenez, who studies obesity and cardiovascular disease at the Mayo Clinic. “Most of the economic analysis we have on bariatric surgery is based on data from the 1990s or early 2000s from patients with very high BMIs.”
In the past, bariatric surgery was only recommended for patients with diabetes and a body mass index (BMI) above 40.
“These are patients who are extremely overweight and who reach a point where it’s nearly impossible to lose weight and keep the weight off by other means,” Lopez-Jimenez said.
But the new guidelines say surgery should also be considered for some mildly obese people with diabetes and a BMI between 30 and 40.
“These guidelines really open up the question of which patients might benefit from surgery,” said Lopez-Jimenez, who reviewed the joint statement, along with Gardner. “Today, you see very few patients with BMIs below 40 having the surgery. But with new techniques that are less aggressive and less intrusive, surgery might really help patients with BMIs in the 30 to 35 range.”
In addition to expanding the criteria of patients who should be considered for surgery, the new guidelines narrowed the type of surgeries that are recommended.
“Some of the more complicated ‘metabolic’ bariatric surgical procedures are better at treating patients with uncontrolled diabetes,” said Gardner. “Other procedures in common use for weight loss, such as Lap-Band surgery, were not advised for patients with diabetes because it didn’t deal with the metabolic problem — the glucose problem — that exists for diabetics.”
The statement concluded that despite the new recommendations, “additional studies are needed to further demonstrate long-term benefits.”
“We need real-life research regarding the safety and effectiveness of the surgeries,” said Lopez-Jimenez. “We need long-term studies of community hospitals doing the surgeries.”
Gardner agreed and said “It’s really important that patients are followed very carefully for five years or more to ensure they aren’t having unexpected problems … It’s one thing to help a very obese patient who weighs 400 pounds lose 100 or 150 pounds, but how that patient is going to do in the long-term remains to be seen.”
Lopez-Jimenez stressed that bariatric surgery isn’t a miracle cure for the growing number of cases of Type 2 diabetes caused by obesity.
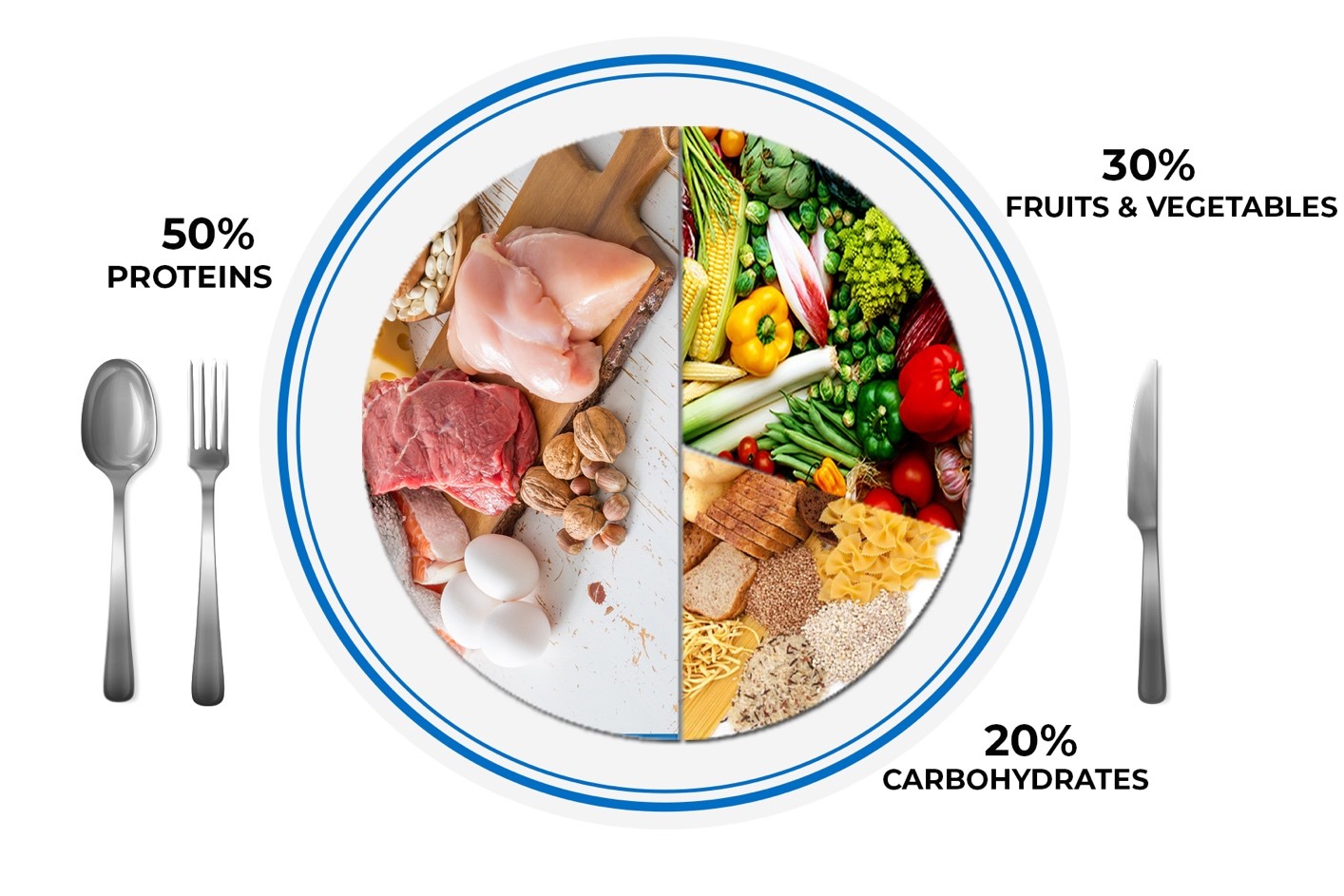
“This should not be seen as a quick fix to eat whatever I want and not exercise,” he said. “These guidelines do not replace a healthy lifestyle … Surgery is recommended only as long as there have been some real attempts to try weight-loss programs. It’s only for when lifestyle and optimal medical therapy have failed.”
Still, Gardner said the guideline changes could change the mindset of both doctors and patients who have run out of other options.
“Patients should look at surgery as a real option, rather than something that’s still theoretical,” Gardner said. “The medical community tends to be pretty conservative about undertaking surgery that has the risk of complications. But I think this scientific validation will encourage a lot of doctors to understand the benefits of this kind of surgery and see it as a valid way to help patients with severe obesity and severe diabetes.”